UC Davis Scientific Symposium Update
February 2024 ADNP Research Update
Written by Kyle Fink, PhD
Written by Kyle Fink, PhD
The Interventional Genetics Team at UC Davis has been working towards the development of three highly novel, targeted therapies for ADNP Syndrome.
On January 25th the UC Davis team, consisting of the Ben-Shalom, Silverman, Segal, and Fink labs conducted a mini-symposium with ADNP Kids Research Foundation of work performed in the last quarter.
The meeting was kicked off by an outstanding Junior Specialist in the Roy Ben-Shalom lab, Ammara Rehman, who showed data from ADNP mouse primary neurons that were grown on Microelectrode Arrays (small dishes with over 26,000 electrodes to measure neuronal function). What Ammara was able to demonstrate is that early on, following growth on these specialized plates, ADNP neurons behaved very differently than neurons isolated from the healthy mice siblings. The ADNP neurons were less active and showed less connections which is common across ASD associated genes.
Very excitingly, Ammara also showed very early pilot data from two of the genetic treatments in these neurons and that the phenotypes, or differences that were observed, seem to be moving back towards the normal level post treatment. While very early in testing and needing more assays to be run, both the phenotypes and early rescue show great promise that the treatments could be effective at restoring neuron function.
Speakers: Katie Lucot, Ammara Rehman, Sara Olgiun, Tomas Salter-Cid, Clair Caputo, Kyle Fink, David Segal, Jill Silverman and Roy Ben-Shalom
On January 25th the UC Davis team, consisting of the Ben-Shalom, Silverman, Segal, and Fink labs conducted a mini-symposium with ADNP Kids Research Foundation of work performed in the last quarter.
The meeting was kicked off by an outstanding Junior Specialist in the Roy Ben-Shalom lab, Ammara Rehman, who showed data from ADNP mouse primary neurons that were grown on Microelectrode Arrays (small dishes with over 26,000 electrodes to measure neuronal function). What Ammara was able to demonstrate is that early on, following growth on these specialized plates, ADNP neurons behaved very differently than neurons isolated from the healthy mice siblings. The ADNP neurons were less active and showed less connections which is common across ASD associated genes.
Very excitingly, Ammara also showed very early pilot data from two of the genetic treatments in these neurons and that the phenotypes, or differences that were observed, seem to be moving back towards the normal level post treatment. While very early in testing and needing more assays to be run, both the phenotypes and early rescue show great promise that the treatments could be effective at restoring neuron function.
Speakers: Katie Lucot, Ammara Rehman, Sara Olgiun, Tomas Salter-Cid, Clair Caputo, Kyle Fink, David Segal, Jill Silverman and Roy Ben-Shalom
Following Ammara’s outstanding talk, an exceptional PostDoc in the Jill Silverman lab, Dr. Sarah Olguin, presented her comprehensive behavioral testing on the ADNP mice. Sarah showed extensive data from a motor, cognitive, and neurophysiology battery in the mice. Several interesting phenotypes, unique to ADNP syndrome, were observed such as a trend of motor dysfunction only in male mice, an assay that reveals increased anxiety, fine motor delays in the gait of the mice, cognitive deficits, and altered sleep patterns. These phenotypes now set the stage for comprehensive behavioral assessments following intervention.
Sarah finished her talk with pilot data collected after testing two of the genetic treatments that were injected into the mice. While the sample size was small and needs to be repeated, there were some signs of rescued motor, anxiety, and cognition in the mice receiving the treatments. The labs are now planning larger studies, in order to more extensively study what differences may be rescued following the targeted interventions.The team will also expand the phenotypes assayed to novel assays such as sleep apneas and evoked potentials, in addition to touchscreen learning and memory.
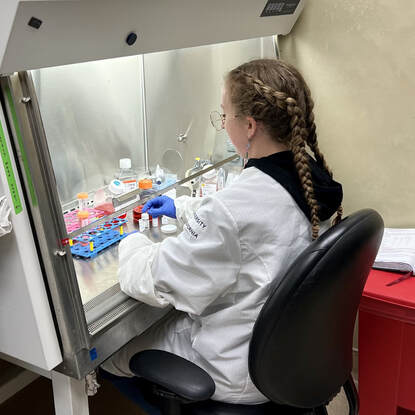
The next speaker was another extremely talented professional scientist from the Fink lab, Dr. Katie Lucot. In her talk, Katie walked through the human cell models that were created for ADNP. The induced pluripotent stem cells were created to mimic the most common mutations found in the ADNP kids and have been successfully converted into neuronal stem cells; with neurons and organoids on the way. Dr. Lucot showed all the validation work to demonstrate the altered RNA and protein levels across the cells as well as described a very novel phenotype that relates to the growth curve of the ADNP cells as compared to the healthy controls.
Katie also did a deep dive on the molecular data and mechanisms for two of the targeted therapies across the mouse cells, mouse brain, and human cell models. Katie finished by describing a novel technique to create more ADNP mutations to broaden our understanding of ADNP Syndrome.
The last talks in the session both came from outstanding graduate students in the lab of Dave Segal; Claire Caputo and Tomas Salter-Cid. Claire started the session by updating the group on the antisense oligonucleotide (ASO) therapeutic intervention that she has been leading with data from human cell models.
The very promising data that she showed has already led to conversations with potential industry partners. Work is now starting with this targeted treatment in the ADNP cell lines that Katie discussed earlier in the day.
The last talk of the UC Davis Mini Symposium came from Tomas Salter-Cid describing a novel mouse model that will be created for these projects. The collaborative labs are each developing a therapy that is highly specific to the human genome. This means for testing in a mouse, we either have to create a second analogous treatment or create a better model system. Tomas covered the second option and discussed the design of a mouse model that would allow for the quick and efficient testing of each targeted therapy without the need to create a ‘mouse’ version. Once this mouse arrives (later this year), the development and validation of each therapy should be greatly expedited.
The Mini-Symposium contained talks from four distinct labs located across the entire UC Davis campus and Medical Campus but demonstrated the highly collaborative and productive environment cultivated by the Interventional Genetics team. Each talk was highlighted by collaboration between all four labs. Mice, cells, genetic treatments, reagents, protocols, and advice flow freely between the groups.
It was very encouraging to see the roughly 25 people all working on ADNP Syndrome all in the same room pushing the different “shots on goal” forward as fast as possible.
On March 5th, the team will be submitting an NIH grant on one of the 3 therapeutics described above to comprehensively assess that single interventional strategy for ADNP Syndrome. While we won’t hear back from NIH until 6 months post-submission, this illustrates that the grant/gift award thus far has placed the team in a more competitive place for state and/or federal funding.
The last talks in the session both came from outstanding graduate students in the lab of Dave Segal; Claire Caputo and Tomas Salter-Cid. Claire started the session by updating the group on the antisense oligonucleotide (ASO) therapeutic intervention that she has been leading with data from human cell models.
The very promising data that she showed has already led to conversations with potential industry partners. Work is now starting with this targeted treatment in the ADNP cell lines that Katie discussed earlier in the day.
The last talk of the UC Davis Mini Symposium came from Tomas Salter-Cid describing a novel mouse model that will be created for these projects. The collaborative labs are each developing a therapy that is highly specific to the human genome. This means for testing in a mouse, we either have to create a second analogous treatment or create a better model system. Tomas covered the second option and discussed the design of a mouse model that would allow for the quick and efficient testing of each targeted therapy without the need to create a ‘mouse’ version. Once this mouse arrives (later this year), the development and validation of each therapy should be greatly expedited.
The Mini-Symposium contained talks from four distinct labs located across the entire UC Davis campus and Medical Campus but demonstrated the highly collaborative and productive environment cultivated by the Interventional Genetics team. Each talk was highlighted by collaboration between all four labs. Mice, cells, genetic treatments, reagents, protocols, and advice flow freely between the groups.
It was very encouraging to see the roughly 25 people all working on ADNP Syndrome all in the same room pushing the different “shots on goal” forward as fast as possible.
On March 5th, the team will be submitting an NIH grant on one of the 3 therapeutics described above to comprehensively assess that single interventional strategy for ADNP Syndrome. While we won’t hear back from NIH until 6 months post-submission, this illustrates that the grant/gift award thus far has placed the team in a more competitive place for state and/or federal funding.